
“Never Events”: What to Know About Health Care Standards and Errors
Jul 10, 2019 Abuse and Neglect
On February 8, 2006, then-President George W. Bush signed the Deficit Reduction Act (DRA) of 2005. This piece of legislation included meaningful changes for Medicare and Medicaid that rippled into our modern health care system.
Notably, the DRA authorized Medicare to refuse higher reimbursements to health care facilities for a variety of serious and preventable medical issues. These Hospital-Acquired Conditions or “Never Events” came to represent ailments that a patient develops when they have received severely deficient medical care.
Any patient who has suffered a “Never Event” at the hands of a health care provider would also be a likely a candidate for a personal injury lawsuit.
What Are “Never Events?”
The national nonprofit organization, National Quality Forum (NQF), first developed a list of “Serious Reportable Events” in 2002. A former CEO at NQF coined the term “Never Events,” which came to be used in its place. The phrase purposefully implies that these events should never happen.
It is important to note that while NQF’s research is supported by Medicare, the list of “Never Events” is not a reflection of Medicare’s reimbursement schedule. Instead, NQF’s list serves as a baseline for the general public on inacceptable standards of health care.
According to NQF, all Serious Reportable Events have three characteristics in common. They are:
- Unambiguous, in that they are clearly identifiable;
- Serious, resulting in death or significant disability; and,
- Usually Preventable, and could be either largely or entirely avoided.
The List of Health Care “Never Events”
NQF’s list currently includes 29 adverse events in seven categories:
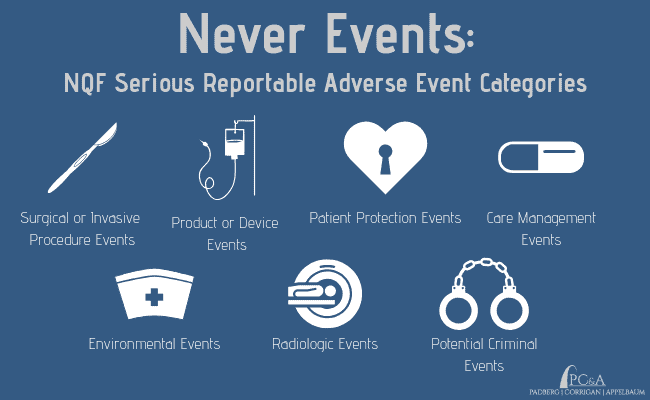
1. Surgical or Invasive Procedure Events
- Surgery or other invasive procedure performed on the wrong site
- Surgery or other invasive procedure performed on the wrong patient
- Wrong surgical or other invasive procedure performed on a patient
- Unintended retention of a foreign object in a patient after surgery or other invasive procedure
- Intraoperative or immediately postoperative/post-procedure death in an ASA Class 1 patient (i.e., a normal and healthy patient)
2. Product or Device Events
- Patient death or serious injury associated with the use of contaminated drugs, devices, or biologics provided by the healthcare setting
- Patient death or serious injury associated with the use or function of a device in patient care, in which the device is used or functions other than as intended
- Patient death or serious injury associated with intravascular air embolism that occurs while being cared for in a healthcare setting
3. Patient Protection Events
- Discharge or release of a patient/resident of any age, who is unable to make decisions, to other than an authorized person
- Patient death or serious injury associated with patient elopement (i.e., disappearance)
- Patient suicide, attempted suicide, or self-harm that results in serious injury, while being cared for in a healthcare setting
4. Care Management Events
- Patient death or serious injury associated with a medication error (e.g., errors involving the wrong drug, wrong dose, wrong patient, wrong time, wrong rate, wrong preparation, or wrong route of administration)
- Patient death or serious injury associated with unsafe administration of blood products
- Maternal death or serious injury associated with labor or delivery in a low-risk pregnancy while being cared for in a healthcare setting
- Death or serious injury of a neonate associated with labor or delivery in a low-risk pregnancy
- Patient death or serious injury associated with a fall while being cared for in a healthcare setting
- Any Stage 3, Stage 4, and unstageable pressure ulcers acquired after admission/presentation to a healthcare setting
- Artificial insemination with the wrong donor sperm or wrong egg
- Patient death or serious injury resulting from the irretrievable loss of an irreplaceable biological specimen
- Patient death or serious injury resulting from failure to follow up or communicate laboratory, pathology, or radiology test results
5. Environmental Events
- Patient or staff death or serious injury associated with an electric shock in the course of a patient care process in a healthcare setting
- Any incident in which systems designated for oxygen or other gas to be delivered to a patient contains no gas, the wrong gas, or are contaminated by toxic substances
- Patient or staff death or serious injury associated with a burn incurred from any source in the course of a patient care process in a healthcare setting
- Patient death or serious injury associated with the use of physical restraints or bedrails while being cared for in a healthcare setting
6. Radiologic Events
- Death or serious injury of a patient or staff associated with the introduction of a metallic object into the MRI area
7. Potential Criminal Events
- Any instance of care ordered by or provided by someone impersonating a physician, nurse, pharmacist, or other licensed healthcare provider
- Abduction of a patient/resident of any age
- Sexual abuse/assault on a patient or staff member within or on the grounds of a healthcare setting
- Death or serious injury of a patient or staff member resulting from a physical assault (i.e., battery) that occurs within or on the grounds of a healthcare setting
The Dangers of Hospital-Acquired Conditions
Patients rely on their doctors, nurses and other medical staff to protect their well-being. Nobody ever expects to be harmed in their care. Unfortunately, one of the reasons “Never Events” are so grave is because they do happen. And these events represent a serious threat to public health.
Hospital-acquired conditions such as septic bedsores are responsible for 90,000 deaths in the United States each year, according to NQF’s December 2011 Fact Sheet. According to the same report, the taxpayer cost of medical harm is equally detrimental, as these conditions translate into $5.7 billion in added expenses. Not included are the extra hospital stays, sleepless nights and countless emotional damages suffered by affected patients and their loved ones.
Filing a Lawsuit for a “Never Event”
Careless mistakes and seemingly insignificant lapses in protocol in a health care facility or nursing home can cause significant harm, and even death. Individuals who have been affected by a “Never Event” or other Hospital-Acquired Condition should contact a personal injury attorney to seek legal recourse.
Depending on the specifics of a given scenario, a “Never Event” could involve different types of litigation, including:
Padberg Appelbaum Knepper (PC&A) is a personal injury law firm located in St. Louis. Our team of attorneys and legal nurse have successfully recovered millions of dollars for innocent victims and their families who were harmed by inadequate medical care.
In one recent case, PC&A attorneys recovered a $4.85 million settlement for an eight-year-old girl who sustained a brain injury resulting from negligent care. After undergoing a Newborn Screen Test, the hospital lost the girl’s results. Her hospital and attending physicians were found liable for a misdiagnosis of congenital hypothyroidism.
If you or a loved one suffered at the hands of a hospital, nursing home or other health care facility, contact the law office of Padberg Appelbaum Knepper for a free consultation with an experienced St. Louis medical malpractice attorney.
